Psychiatric Care AR
Designing augmented reality interactions to make psychiatric care safer
Pulse uses low-power radar to protect people at the most vulnerable time in their lives. It maps high-risk areas in psychiatric wards and alerts staff when a dangerous situation occurs, enabling timely intervention and reducing unattended medical emergencies, self-harm, and suicide.
Role
As a freelance product designer, I led design development with Safehinge Primera toward market deployment and product validation. This included primary research, product roadmapping and value-proposition development, UX and design-system definition, prototyping, and WCAG-compliant interfaces.
Deliverables
Product roadmap
UI & UX design
WCAG compliance
Design system
Outcomes
First commercial version designed
Future feature roadmap established
Product trials initiated
Respectful Patient
Safety Monitoring
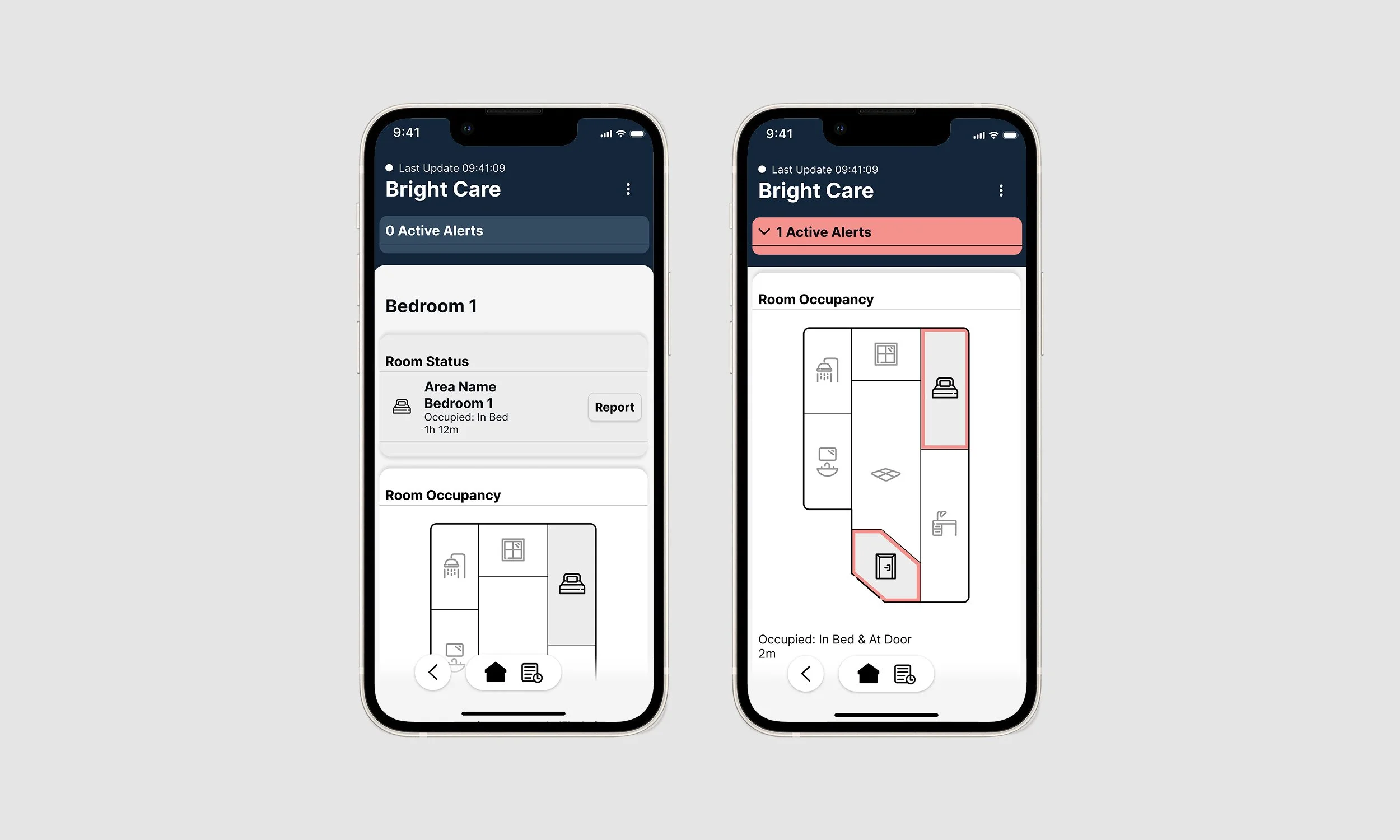
Unlike camera-based systems, radar offers a balanced approach to delivering critical location and safety information without compromising privacy. The interface intentionally limits occupancy detail, using colour cues and alert triage to focus care workers' attention on areas that require immediate support.
The design was shaped by auditing existing proof-of-concept systems, creating a new triage framework to handle various alert types, and prototyping multiple concepts for evaluation. A final system was then developed, incorporating feedback from testing.
Response Coordination
& System Readiness
To improve alert visibility, a ward office portal was developed. It displays alert locations within the ward layout, helping staff coordinate responses more effectively. The system also monitors active staff handsets to ensure teams on the ground maintain continuous data access so they can respond effectively.
In building the portal, existing customer ward plans were analysed, and a range of visualisation concepts was developed. These were assessed for utility, and the final framework was pressure-tested against all known configurations to ensure robustness and scalability.
Algorithm Training
& System Improvement
To continuously improve algorithm accuracy and reliability, a training mechanism was built into the interface. This allowed staff to quickly categorise inaccurate alerts at the point of dismissal, feeding data back into the system for ongoing refinement and model training.
Developing this mechanism involved close collaboration with the data science team to map all conceivable scenarios that could produce inaccurate data. This was consolidated into a feedback information architecture designed to preserve response times for critical alerts.
Project Data
User need
At the lowest moment of a person’s life, they may attempt suicide or enter a state where they are unable to care for themselves.
Context
Psychiatric wards in the UK help service users re-establish stable mental states and care routines so they can return to community settings. Many arrive in crisis and require close monitoring to prevent harm during stabilisation.
Value proposition & business case
Continuous observation (restrictive practice) strains staffing and impacts patient autonomy and privacy. A non-invasive monitoring solution can reduce the need for direct observation, improving safety, dignity, and staff efficiency.
Technologies
Restrictive practice techniques; Low-power radar sensors; IOT and edge infrastructure; smartphone application; monitoring dashboard.